When people start noticing unusual sensations such as squeaking, grinding, clicking, or popping in the hip, it can feel unexpected or insignificant — something to ignore or joke about. Yet the hip is one of the most heavily used weight‑bearing joints in the body, designed to move smoothly and support daily activities like walking, standing, and climbing stairs. These noises often signal that the normally smooth cartilage lining the joint is not functioning optimally, allowing friction and irritation between surfaces that should glide without resistance. This friction can irritate surrounding tissues, subtly alter how the hip moves, and contribute to pain or stiffness over time. While an occasional sound without pain can be benign, consistent noise accompanied by discomfort or reduced mobility may indicate underlying problems such as early‑stage hip osteoarthritis, a labral tear, hip impingement, or other structural issues within the joint. Recognizing these cues early gives people an opportunity to protect long‑term joint health, preserve mobility, and reduce the risk of progression to more severe symptoms, rather than dismissing the signs as “just a noise.”
Medical evaluation is one of the most important steps when hip sensations become recurring or painful. Many people delay seeking help because discomfort may come and go, or because they assume joint problems only occur in older age — but that isn’t always true. Joint issues can affect individuals of all ages, especially those who are physically active, have experienced prior injuries, or whose daily routines involve prolonged sitting or repetitive movements. Clinicians such as orthopedic doctors or sports medicine specialists can assess hip function through physical examinations and, when needed, imaging tools like X‑rays or MRI scans to identify conditions such as cartilage thinning, inflammation, impingement, or labral tears — a tear of the cartilage ring that surrounds and stabilizes the hip socket that often causes clicking or catching sensations. Early identification matters because many treatment options — such as guided physical therapy, activity modification, and targeted exercises — are more effective when damage is minimal. Waiting too long can allow minor issues to worsen, increasing the likelihood of chronic pain or the need for more invasive interventions. Seeking medical evaluation is not an overreaction; it’s a proactive step in understanding one’s body and protecting functional movement for the future.
Lifestyle choices significantly influence how the hip joint ages and responds to daily stress. Body weight is a particularly impactful factor because the hips bear much of the body’s load with every step. Research shows that even modest weight loss can disproportionately reduce mechanical stress on the joint during regular activities, helping ease discomfort and slow cartilage wear. Beyond weight management, daily habits such as prolonged sitting, poor posture, or wearing shoes without adequate support can subtly alter hip mechanics, increasing strain on joint structures. Simple adjustments — such as taking frequent breaks from sitting, maintaining neutral posture, and choosing supportive footwear — can help the joint move more naturally and reduce unnecessary stress. Nutrition also plays a role, as a balanced, nutrient‑rich diet supports overall tissue health, muscle strength, and inflammation control. Although no specific food can “fix” a joint problem, consistent healthy habits create an internal environment that helps the body manage stress and repair itself more effectively. Over time, these small lifestyle shifts can make a meaningful difference in comfort and mobility.
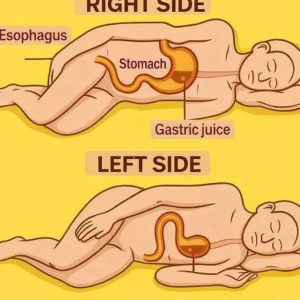
Movement itself poses both challenges and opportunities for hip health. High‑impact activities that involve repetitive pounding, sudden direction changes, or deep compression — such as running on hard surfaces, jumping, or heavy squats — can exacerbate symptoms when the joint is already irritated. This doesn’t mean all movement should stop; in fact, avoiding activity entirely can weaken the muscles that support the hip and reduce joint lubrication, making symptoms worse. The key is to choose joint‑friendly forms of exercise that promote mobility without excessive strain. Low‑impact activities like swimming or water‑based exercises are excellent because the water supports body weight while allowing a full range of motion. Cycling, whether on a stationary bike or outdoors, provides cardiovascular benefit with minimal hip impact. Walking at a comfortable pace on flat, even surfaces helps maintain circulation and joint motion without overloading the joint. These activities support joint health by encouraging healthy movement patterns, improving endurance, and benefiting mental well‑being, all while minimizing the risk of aggravating existing hip issues.
Muscle strength and balance are critical components of hip health that are often overlooked until pain develops. The hip doesn’t operate in isolation — it relies on the surrounding muscles, including the glutes, core, and thigh muscles, to stabilize and guide movement. When these muscles are weak or poorly coordinated, the hip joint itself takes on extra stress, accelerating wear and potentially leading to discomfort, reduced range of motion, or compensatory movement patterns that affect other joints. Strengthening supportive muscles helps distribute forces more evenly across the hip and improves alignment during everyday activities like walking, standing, and lifting. Exercises such as bridges, side‑lying leg raises, and controlled hip movements activate key stabilizers when performed correctly. A physical therapist can design a personalized program to address specific weaknesses, movement patterns, and flexibility needs — an important safeguard because incorrect technique may cause more harm than benefit. Gradual, consistent strengthening not only reduces pain but also builds confidence in movement, making it easier to stay active and engaged in life. Importantly, building strength isn’t about pushing through pain; it’s about creating stability and resilience through thoughtful, sustainable practice.
Long‑term hip health is shaped by attention, patience, and informed decision‑making. A squeaking, clicking, or uncomfortable hip should not be ignored, but it also doesn’t have to limit someone’s future activity. Many people successfully manage early joint symptoms by combining medical guidance, appropriate lifestyle adjustments, joint‑friendly exercise, and strength training. Attentive listening to one’s body and responding early can preserve mobility and independence for years to come. Joint health is not just about avoiding pain — it’s about maintaining the ability to move freely, participate in meaningful activities, and support overall well‑being. Small, consistent efforts often matter more than dramatic interventions. By taking symptoms seriously, seeking professional input when needed, and making thoughtful choices, individuals can empower themselves to protect their hips and maintain an active, balanced life. The body has a remarkable capacity to adapt when supported properly, and caring for hip joints today can help ensure comfort and confidence in movement well into the future.