Waking up in the middle of the night is something nearly everyone experiences at some point, but when it becomes frequent it can have a meaningful impact on daily functioning and well‑being. Interrupted sleep often leads to feelings of grogginess, irritability, and difficulty concentrating the following day, and over time those disruptions can even weaken immune function and make the body more vulnerable to illness. While occasional nighttime awakenings are normal — humans naturally cycle through sleep stages — repeatedly waking up may signal that something in your routines, environment, or health needs attention. The good news is that many common causes of sleep disruptions are manageable with thoughtful adjustments to behavior, sleep habits, and the bedroom environment.
To address nighttime awakenings, it helps first to understand what contributes to them. Several lifestyle factors — like drinking caffeine later in the day, consuming alcohol close to bedtime, eating heavy or spicy meals in the evening, or taking long afternoon naps — can all fragment sleep. Caffeine, for example, blocks adenosine, a chemical that helps promote sleepiness, and can continue to affect the brain hours after it’s consumed. Alcohol might help some people fall asleep initially, but as it wears off it can cause the sleep cycle to fragment, leading to mid‑night awakenings. Medical factors such as sleep apnea, restless legs syndrome, chronic pain, hormonal changes, or frequent urination at night can also disrupt sleep and may warrant medical evaluation if they’re persistent. Being aware of these triggers clarifies why waking up at night feels difficult to control — it’s often the result of multiple small influences adding up.
The sleep environment plays a powerful role in how easily you stay asleep through the night. Experts recommend keeping the bedroom cool, dark, and quiet, with temperatures around 60–67°F (15–19°C) to support deeper, uninterrupted rest. Light — especially bright or blue light from screens — can suppress melatonin, the hormone your body produces to regulate sleep cycles, so minimizing exposure before bedtime and during nocturnal wakeups can make it easier to fall back asleep. Blackout curtains, white noise machines or fans, and a comfortable mattress and bedding help cue the brain that the bedroom is a sleep‑only space, not a place for stimulation or wakeful thinking. Even small environmental irritants — like dust, poor air quality, or room odor — may cause micro‑arousals, so maintaining good ventilation and cleanliness also contributes to restful sleep.
Emotional state and stress levels heavily influence nighttime rest. A racing mind or unresolved thoughts can pull you awake or make it hard to fall back asleep once disturbed. Research suggests that stress hormones like cortisol can rise during the night, especially between the early morning hours, making the brain more alert and prone to awakening. Creating a wind‑down routine before bed — such as journaling worries earlier in the evening, practicing slow breathing, light stretching, or gentle meditation — helps ease mental tension and signals to your body that it’s time to relax. The NHS recommends that if you wake and can’t sleep for about 20 minutes, getting out of bed and doing a quiet, relaxing activity in dim light (like reading a calming book or sipping herbal tea) can teach your brain that bed is for sleep, not wakefulness. Over time, these practices reduce anxiety around sleep and can lessen nighttime wake‑ups.
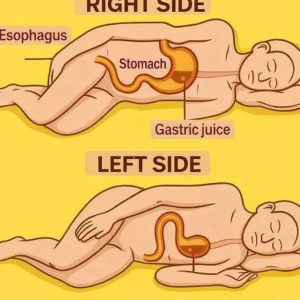
Daily habits outside of bedtime matter just as much as what you do in the evening. Consistency in your sleep schedule — going to bed and waking up at the same times every day — helps regulate your internal clock, making uninterrupted sleep more likely. Avoiding large meals close to bedtime prevents digestive discomfort or acid reflux that can jerk you awake, and limiting fluids in the two hours before bed can reduce nocturnal bathroom trips. Regular physical activity earlier in the day promotes deeper sleep at night, though vigorous exercise too close to bedtime can have the opposite effect by elevating adrenaline and alertness. It’s also important to consider medication side effects; certain prescription drugs, including some antidepressants, steroids, and beta blockers, are known to interfere with sleep patterns, and discussing alternatives with a healthcare professional could be helpful.
When practical adjustments and good sleep hygiene — like avoiding screens before bed, reducing stimulants, cooling the room, and keeping a consistent schedule — aren’t enough, it’s worth considering whether an underlying sleep disorder or health condition might be at play. Conditions such as obstructive sleep apnea, arthritis pain, restless legs syndrome, bladder dysfunction, or even seasonal hormonal shifts can cause persistent sleep interruptions that don’t respond to lifestyle tweaks alone. In these cases, consulting a healthcare provider or sleep specialist can help diagnose the issue accurately and recommend appropriate treatment or therapies such as cognitive behavioral therapy for insomnia (CBT‑I), which has been shown to reset sleep patterns and reduce frequent awakenings.
Ultimately, waking up in the middle of the night doesn’t have to be a permanent struggle, and small, thoughtful changes can lead to meaningful improvements. By paying attention to sleep patterns, identifying lifestyle contributors, optimizing your environment, and tending to emotional well‑being, you create conditions that support deeper, more restorative sleep. While occasional nights of disrupted sleep are normal, consistent interruptions that affect daily functioning may require professional support. With patience and steady adjustments, it’s possible to reduce nighttime wakefulness and enjoy quieter nights and brighter mornings.